The Critical Impact of Cortisol on Ovulation and Sperm Quality: Your Guide to Reducing Stress for Conception
Introduction (The Hidden Barrier to Pregnancy)
Many couples find themselves in a bewildering state: physically healthy, committed to conception, yet unable to achieve pregnancy. They navigate countless cycles, diagnostic tests, and mounting emotional pressure, only to hear the frustrating phrase, “unexplained infertility.”
The truth is, the true barrier often isn’t structural or pathological—it’s hormonal, invisible, and rooted in the modern nervous system.
Why are successful couples still struggling to conceive despite no physical diagnosis? The invisible enemy: high stress hormones and fertility.
We often dismiss chronic stress as “just part of life,” yet its physiological consequence—elevated cortisol—is a potent disruptor of reproductive health in both sexes. This chemical signal, designed for ancient survival, actively suppresses the systems required for a baby.
This guide breaks down the little-known physiological impact of cortisol on ovulation and sperm quality and provides a comprehensive, six-part strategy to overcome this hormonal barrier. We will move past the vague advice of “just relax” and provide actionable, science-backed insights into the cortisol-progesterone link and its role in disrupting the cycle.
High cortisol is not just an indicator; it is a key player in psychological stress, infertility, and understanding its mechanism is the first step toward conception.
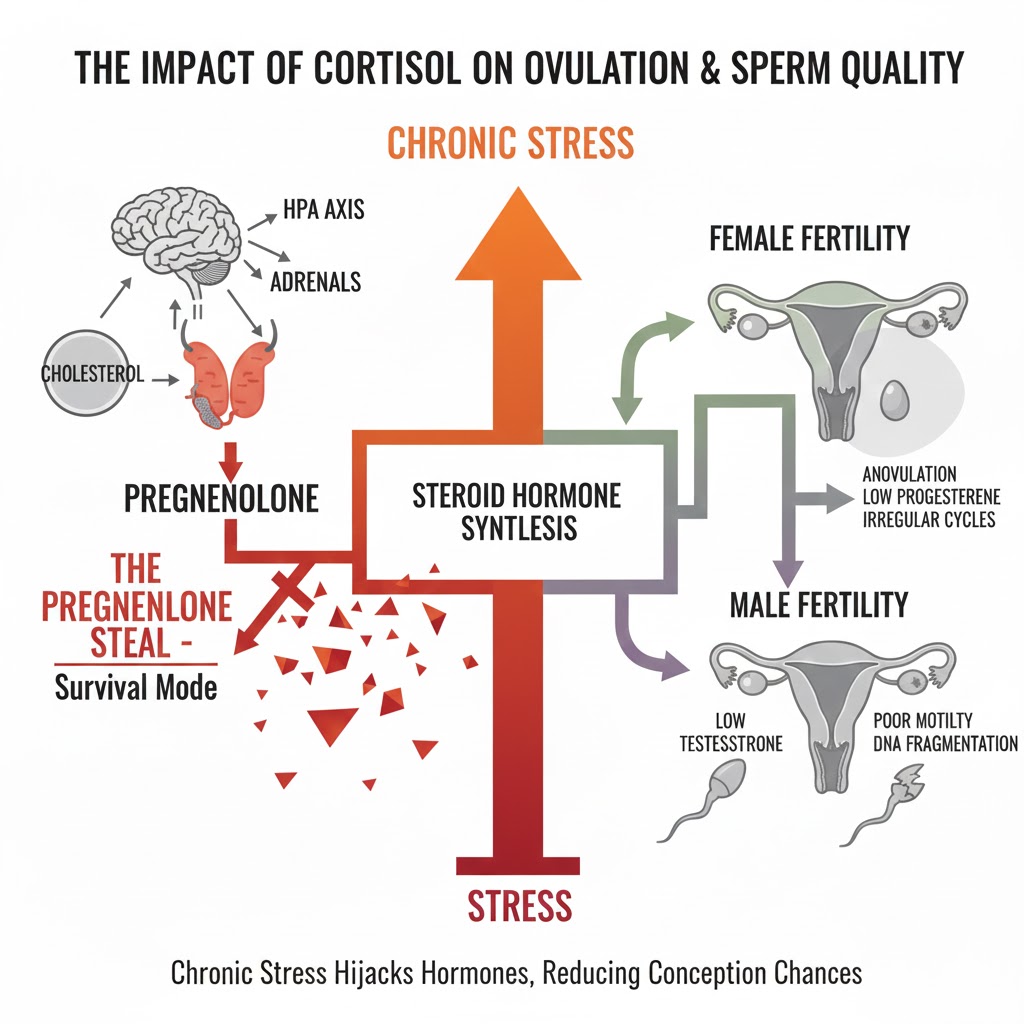
Secret 1 – The ‘Pregnenolone Steal’ and Progesterone Crash
Why High Cortisol Triggers Progesterone Deficiency and Anovulation
To understand how stress sabotages fertility, we must first recognize the body’s ironclad priority: survival always precedes reproduction. When we perceive stress—whether it’s a physical threat or a demanding job—the body initiates an emergency response managed by the adrenal glands.
Understanding the HPA Axis and the Fight-or-Flight Cascade
The entire process begins in the brain with the Hypothalamic-Pituitary-Adrenal (HPA axis). When a stressor occurs, the hypothalamus releases corticotropin-releasing hormone (CRH), signaling the pituitary gland, which in turn signals the adrenal glands to pump out cortisol.
This cascade is meant to be acute, providing a burst of energy and focus. However, chronic stress keeps the HPA axis perpetually “on,” flooding the bloodstream with glucocorticoids.
Cortisol, the body’s primary glucocorticoid, is essential for life, helping to regulate blood sugar, inflammation, and blood pressure. The problem arises when this hormone is produced continuously, placing an overwhelming demand on the adrenal system.
This constant demand for cortisol creates a hormonal bottleneck at the very start of the sex hormone synthesis pathway.
The Pregnenolone Steal Explained: When Cortisol Robs Reproduction
All steroid hormones—including cortisol, estrogen, progesterone, and testosterone—begin with cholesterol. Cholesterol is converted into pregnenolone, which is often referred to as the “mother hormone.” From pregnenolone, the pathway splits, leading either toward cortisol production or toward the reproductive hormones.
When the HPA axis is active due to chronic stress, the body institutes a critical survival mechanism known as the Pregnenolone Steal. To ensure the immediate survival demands are met, the body aggressively shunts pregnenolone down the cortisol pathway. This action literally robs the reproductive pathways of their essential precursor.
The most immediate casualty of the Pregnenolone Steal is progesterone. This results in a clinical and functional progesterone deficiency.
Progesterone is crucial for fertility; it stabilizes the uterine lining after ovulation, making the endometrium receptive to implantation. It is also responsible for maintaining a pregnancy in the early weeks.
When progesterone levels crash, the body cannot sustain a healthy environment for an embryo. This direct cortisol progesterone link is why many women experience luteal phase defects or recurrent early losses.
The resulting progesterone deficiency and why it leads to a failure in the uterine lining is a core component of psychological stress infertility. By understanding this physiological prioritizing, we can see exactly why reducing the cortisol load is non-negotiable for successful conception.
Fertility – Sabotaging the Menstrual Cycle
The Direct Impact of Cortisol on Ovulation and Irregular Periods
The continuous signal of high cortisol does more than just deplete progesterone reserves; it directly interferes with the finely tuned signals required for the menstrual cycle to function properly.
Suppressing the Luteinizing Hormone (LH) Surge
The reproductive cycle is governed by the Hypothalamic-Pituitary-Gonadal (HPG axis), the hormonal counterpart to the HPA axis. When cortisol is high, the hypothalamus perceives this as an environmental threat.
The hypothalamus, being highly conservative, determines that if the environment is too stressful for the mother to survive, it is certainly too dangerous to sustain a pregnancy.
To shut down reproduction, the stress hormones directly inhibit the release of Gonadotropin-Releasing Hormone (GnRH), the master signal for the HPG axis.
A suppressed GnRH signal means the pituitary gland cannot adequately produce the Follicle-Stimulating Hormone (FSH) necessary for follicular development, nor can it generate the critical Luteinizing Hormone (LH) surge required for the mature egg to burst forth.
The consequence is a failure of the ovulation function, resulting in what is termed anovulation stress. This isn’t just about missing a period; it means the entire ovulation attempt has been derailed due to the body’s constant stress signal.
Even when a cycle is not fully skipped, the increased levels of cortisol can still compromise the quality of the ovulated egg, impacting the optimal environment within the follicular fluid.
The Danger of High-Stress Irregular Periods
While full anovulation is the most dramatic consequence, even subtle disruptions are damaging. Discusses how high-stress irregular periods signal hormonal imbalance, presenting as cycles that are either slightly shorter, longer, or less vigorous than optimal.
These subtle shifts—driven by elevated cortisol—can significantly affect the timing and duration of the fertile window.
For couples tracking their cycle meticulously, these subtle hormonal shifts can make timing intercourse or IUI procedures exceptionally difficult. Even small delays or variations in the cycle length due to stress can mean they are missing the crucial 12–24 hour window of peak fertility.
Moreover, chronic stress ensures the internal environment remains pro-inflammatory, which is detrimental to implantation, even if a fertilized egg is present. Addressing the underlying stress is therefore key to restoring the predictable, robust ovulation function necessary for successful conception.
Male Fertility – Protecting Sperm Quality
The Impact of Cortisol on Sperm Quality: Motility and DNA Fragmentation
Fertility is a shared responsibility, and the detrimental impact of cortisol on ovulation and sperm quality affects both partners equally. While the female cycle is acutely sensitive to hormonal changes, the male reproductive system, particularly sperm production, is heavily reliant on a stable, non-inflammatory environment that high stress aggressively undermines.
Cortisol’s Direct Attack on Sperm Count and Motility
Just as cortisol diverts resources from female hormones, it also competes with and inhibits the production of testosterone in men. Testosterone is the primary driver of spermatogenesis (sperm production). The relationship between high cortisol and reduced cortisol and testosterone levels in men is well-established; the higher the stress, the lower the anabolic (building) hormone.
How stress hormones cause a visible stress decrease in sperm count is twofold:
- Reduced Production: Lower testosterone means a slowdown in the factory floor of the testes, leading to fewer sperm being created overall.
- Impaired Maturation: The sperm that are produced often suffer from quality issues, resulting in suboptimal sperm motility (the ability to swim effectively) and abnormal structure (sperm morphology). Sperm need energy and an ideal environment to move, and the systemic inflammation driven by cortisol depletes that energy and damages the necessary structures. This significantly lowers the chances of fertilization.
The Threat of Oxidative Stress Sperm DNA Damage
Perhaps the most insidious damage cortisol inflicts on male fertility is via oxidative stress. Why elevated glucocorticoids increase free radicals is simple: chronic high cortisol increases cellular metabolic activity and inflammation throughout the body. The semen is no exception. This cascade creates a hostile environment, leading to oxidative stress and sperm DNA damage.
Oxidative stress is essentially “rust” on the sperm cell. This damage can manifest as significant sperm fragmentation, meaning the genetic material within the sperm is broken or damaged.
Even if this sperm manages to fertilize an egg, high sperm fragmentation drastically reduces the chance of successful implantation and increases the risk of early miscarriage. This silent damage is a primary contributor to male-factor infertility, often overlooked by basic semen analysis.
Therefore, mitigating the impact of cortisol on sperm quality is a foundational step in optimizing male fertility, focusing specifically on reducing the systemic oxidative burden.
Diagnostic Clarity – Testing Your Stress Load
Testing for High Cortisol: The First Step to Taking Control
We cannot manage what we do not measure. For couples dealing with unexplained fertility challenges, getting an objective measure of the chronic stress load is the critical next step. However, standard diagnostics are often inadequate.
Traditional morning blood draws only capture a single snapshot, usually the peak, and are immediately skewed by the stress of driving to the lab or even the needle poke itself.
They completely miss the diurnal rhythm—how cortisol should rise in the morning (the ‘cortisol awakening response’) and steadily decline throughout the day, hitting its lowest point before sleep. When this rhythm is flat or inverted, it is a key sign of chronic adrenal dysfunction and high psychological stress infertility.
The Gold Standard: Why the Salivary Cortisol Test is Key
The salivary cortisol test is the gold standard for measuring the body’s true stress footprint. Why traditional blood tests often miss chronic stress and why the salivary cortisol test is superior for measuring free cortisol over 24 hours is because saliva measures the unbound or biologically active cortisol that is free to enter cells and exert its effects.
By collecting samples at four points (morning, noon, evening, and before bed), the test maps the HPA axis rhythm, revealing if it is exhausted, constantly elevated, or simply deregulated.
Interpreting your results and knowing when to seek professional guidance is crucial, as the pattern is often more important than a single number. For instance, high evening cortisol is a major red flag, as it signals the body is too “on” to rest and recover, perpetually fueling the Pregnenolone Steal.
Addressing these high cortisol patterns has shown measurable improvements in IVF outcomes and stress. Research suggests that patients who engage in stress reduction programs before or during IVF cycles have higher success rates.
Recognizing and quantifying your high cortisol symptoms—such as morning fatigue, afternoon energy crashes, and “wired but tired” insomnia—and linking them to the hormonal pattern revealed by the salivary cortisol test provides the necessary data to build a targeted, effective treatment plan.
The Six-Part Strategy – Natural Ways to Lower Cortisol (The Secret 6)
6 Natural Ways to Lower Cortisol Levels to Conceive
Once you understand the profound impact of cortisol on ovulation and sperm quality, the next step is implementing a focused strategy to downregulate the stress response. These six strategies are the foundation of natural ways to lower cortisol and restore HPA axis balance.
1. Targeted Supplementation
Supplements provide the raw materials needed to help the overworked adrenal glands recover and replenish. The Best Supplements for High Cortisol include:
- Magnesium: Known as nature’s tranquilizer, magnesium calms the nervous system and is consumed rapidly by the body during stress. Supplementing can help the nervous system switch from sympathetic (fight-or-flight) to parasympathetic (rest-and-digest) dominance.
- B-Complex: The B vitamins are crucial cofactors in adrenal hormone production and metabolism. They support healthy nerve function and cellular energy, which are both drained by chronic stress.
- Vitamin C: The adrenal glands are one of the body’s highest repositories of Vitamin C, which is essential for cortisol synthesis. Chronic stress depletes these stores, making supplementation necessary for overall adrenal health.
2. Harnessing Adaptogens for Stress Relief
Adaptogens are natural compounds that help the body adapt to stress by modulating the HPA axis, normalizing cortisol levels, whether they are too high or too low. Key insights into using Adaptogens for stress safely during conception include:
- Ashwagandha: This root is perhaps the best-studied adaptogen for stress. It has been shown in clinical trials to significantly reduce serum cortisol levels and combat the symptoms of chronic stress.
- Rhodiola: Ideal for individuals suffering from brain fog and fatigue, Rhodiola helps improve mental performance under stress and strengthens the body’s resistance to physical and emotional burnout. Always consult with a healthcare provider before starting adaptogens, especially when trying to conceive.
3. Sleep as a Hormone Regulator
Sleep is not a luxury; it is the body’s nightly hormone factory reset. The vital connection between consistent, quality sleep and balancing your stress hormones and fertility cannot be overstated.
Cortisol is regulated on a 24-hour cycle (circadian rhythm), and sleep disruption is a massive physical stressor that immediately raises cortisol. Prioritize seven to nine hours of consistent, deep sleep, aiming to be asleep by 10:30 PM, to align with natural hormonal cycles.
4. Mind-Body Practices
Mind-body techniques are not just relaxation methods; they are direct tools to regulate the nervous system. Integrating mindfulness and fertility techniques (meditation, yoga) to downregulate the HPA axis teaches the body that it is safe, which is the exact opposite signal of high cortisol.
Daily practices like deep, diaphragmatic breathing or spending 10 minutes in non-judgmental meditation can literally shift the brain chemistry away from the stress response.
5. Exercise Re-defined
While exercise is healthy, high-intensity interval training (HIIT) and excessive long-distance running can be physical stressors that spike cortisol, worsening the cortisol progesterone link and causing further stress, decreasing sperm count.
The goal is switching from high-intensity stress to restorative movement. Opt for resistance training (which supports testosterone and bone health) and gentle exercises like walking, swimming, or restorative yoga to promote circulation without triggering a cortisol spike.
6. Diet Adjustments
Diet plays a crucial role in regulating cortisol via blood sugar stability. Avoid simple carbohydrates, excessive caffeine, and refined sugar, as they cause sharp blood sugar spikes and crashes. These crashes trigger an emergency cortisol release to stabilize glucose, keeping the HPA axis engaged.
Focus on whole, nutrient-dense foods, balanced macronutrients (protein, healthy fats, complex carbs), and sufficient water intake. These combined strategies provide a holistic answer to how to lower cortisol to conceive.
Does chronic stress cause infertility, or just make it harder to conceive?
While stress alone may not be the root cause of all infertility, there is strong evidence that psychological stress is a real and common barrier. Chronic stress directly impacts the HPG axis, causing hormonal imbalances like progesterone deficiency and disrupting the essential chemical cascade needed for both egg and sperm development. It doesn’t cause irreparable physical damage, but it does create a physiological environment hostile to conception, making it significantly harder to achieve and sustain pregnancy.
What is the overall impact of cortisol on ovulation and sperm quality?
The full impact of cortisol on ovulation and sperm quality is a systemic disruption. In women, it primarily causes anovulation stress and low progesterone via the Pregnenolone Steal. In men, it lowers testosterone, which results in reduced sperm motility and increased oxidative stress, and sperm DNA damage. Addressing cortisol is critical for optimizing both sides of the conception equation, ensuring both the quantity and quality of reproductive material are at their peak.
What is the single fastest way to see an improvement in my cortisol levels?
The single most effective, free strategy is optimizing deep, consistent sleep. Lack of sleep is a massive physical stressor that keeps cortisol elevated. Disruptions to the circadian rhythm are immediately reflected in a dysfunctional HPA axis pattern. Combining improved sleep (in bed by 10:30 PM, dark room) with targeted use of powerful adaptogens for stress (like Ashwagandha) can often yield quick results in measurable cortisol reduction, especially in the evenings.
I have high stress, but my periods are regular. Could cortisol still be an issue?
Yes. Even with regular cycles, high cortisol can affect the quality of the egg and the receptivity of the uterine lining (due to the Pregnenolone Steal). A regular cycle confirms that the structural timing is present, but it says nothing about the hormonal vigor. Furthermore, in men, the impact of cortisol on sperm quality can be severe, causing issues with motility and DNA fragmentation, even if the woman’s cycle appears normal. Addressing the stress load is a benefit to both partners.